Chronic ocular hypotony: Moorfields Eye Hospital trials new treatment approach
The management of chronic ocular hypotony remains a significant challenge. A new study by clinical researchers at University College London (UCL) and Moorfields Eye Hospital now demonstrates the effectiveness of a widely used intravitreal injection in treating this rare condition.
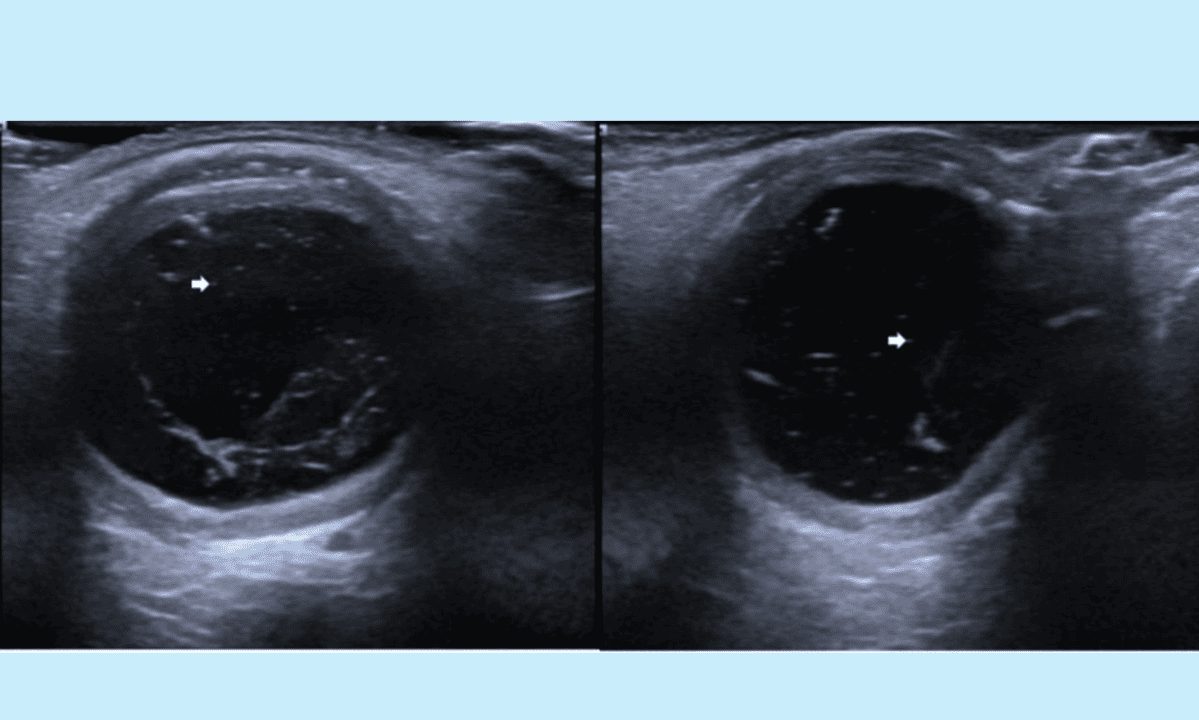
Hypotony is characterised by abnormally low intraocular pressure (IOP) of <6.5 mm Hg, which alters the eye’s normal shape and internal structure. Over time, this can lead to progressive and permanent vision loss, often taking several years to result in blindness. Hypotony may develop as a result of underlying eye conditions that damage the part of the eye responsible for producing the fluid that maintains normal eye pressure.
Until now, the standard treatment for eyes losing vision from low pressure has been to fill them with silicone oil. This has many benefits but is not ideal as it can be toxic to eye structures over long periods of time and is difficult to see through.
The data published in the British Journal of Ophthalmology indicates that intravitreal hydroxypropyl methylcellulose (HPMC) can be safely used to increase the volume of eyes with hypotony, increasing both their size and pressure. Intravitreal viscoelastic agents have been used anecdotally to manage hypotony, but no structured protocols or prospective data have been published.
Remarkably, in addition to restoring the eye’s anatomy, patients also regained sight. Seven of the eight patients who received the treatment experienced improvements in vision, eye pressure and length restoration after a twelve-month course of treatment. These all came from the world’s first dedicated hypotony clinic, enabled by funding from Moorfields Eye Charity. These findings suggest a reproducible therapeutic strategy with potential to prevent irreversible ocular damage in eyes with visual potential.
Moorfields consultant ophthalmologist Harry Petrushkin, lead author of the study, said: “We are excited that this simple treatment has proved so effective for patients with this rare condition. This is the start of a process of understanding more about the balance of fluid inside the eye, leading to improved care for our patients.”
Co-author Professor Gus Gazzard (UCL Institute of Ophthalmology and Moorfields Eye Hospital) commented: “This is a truly transformative new therapy that brings hope to patients otherwise without options, for what was previously an untreatable blinding and disfiguring condition. This robust proof of principle study has already exceeded my hopes of what sight recovery might be achievable.
“I hope that we shall be able to make it more widely available to more patients very soon, but of course these are early steps, and more hard work will be needed, not least to raise the funds needed to optimise this treatment.”
Source: Moorfields Eye Hospital