US scientists test surgical technique to improve cell therapy for dry AMD
National Institutes of Health (NIH) scientists have developed a new surgical technique for implanting multiple tissue grafts in the eye's retina. The findings in animals may help advance treatment options for dry age-related macular degeneration (AMD).
A report about the technique was published in JCI Insight.
In diseases such as AMD, the retina tissue degenerates. Scientists are testing therapies for restoring damaged retinas with grafts of tissue grown in the lab from patient-derived stem cells. Until now, surgeons have only been able to place one graft in the retina, limiting the area that can be treated in patients, and as well as the ability to conduct side-by-side comparisons in animal models. Such comparisons are crucial for confirming that the tissue grafts are integrating with the retina and the underlying blood supply from the choriocapillaris.
For the technique, investigators designed a new surgical clamp that maintains eye pressure during the insertion of two tissue patches in immediate succession while minimizing damage to the surrounding tissue.
In pig models of laser-induced outer retinal degeneration, the scientists used their newly designed surgical technique to compare two different grafts placed sequentially in the same experimentally induced AMD-like lesion: a patch of induced pluripotent stem cell–derived retinal pigment epithelium (iRPE), matured on a biodegradable poly(lactic-co-glycolic acid) (PLGA) scaffold, and a control patch consisting of the PLGA scaffold alone.

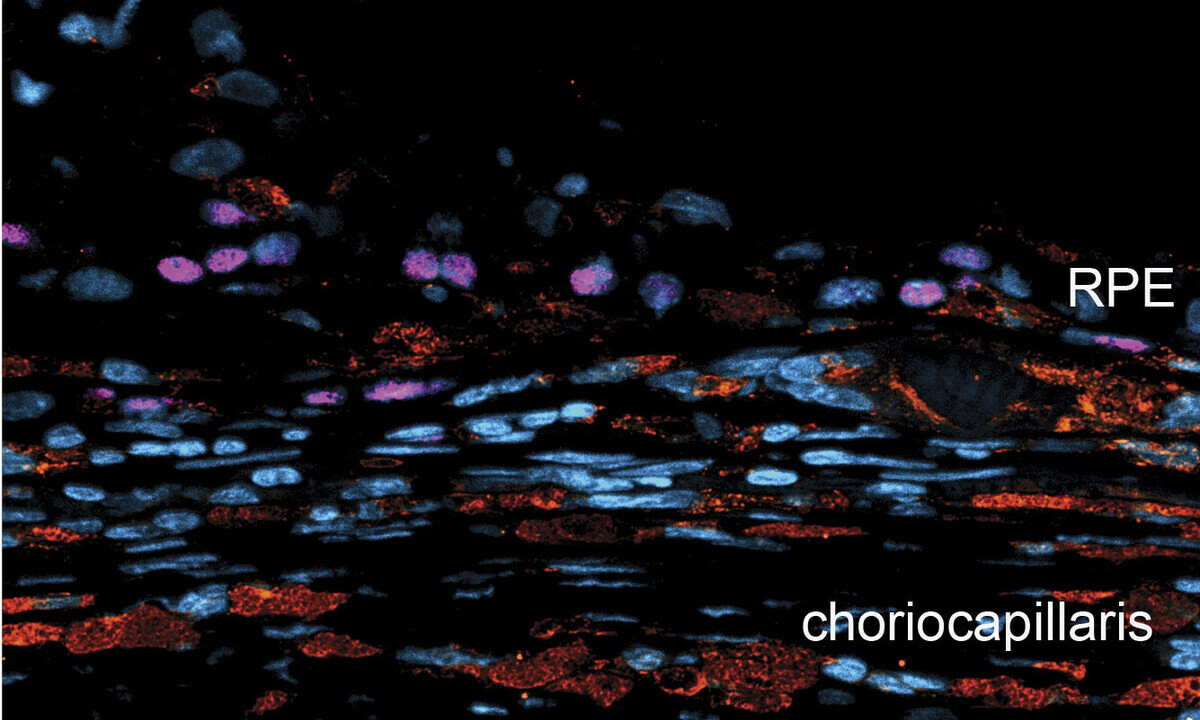
Top image shows retina transplanted with empty scaffold, which served as a control. Bottom image shows how the stem cell-RPE graft (labeled pink) shows regeneration of choriocapillaris (labeled red), the part of the eye that supplies the retina with oxygen and nutrients. Credit: Kapil Bharti, Ph.D.
Post surgery, scientists used artificial intelligence to analyze retinal images and compare the effects of each graft. They observed that the RPE grafts promoted the survival of photoreceptors, while photoreceptors near scaffold-only grafts died at a much higher rate. Additionally, they were able to confirm for the first time that the RPE graft also regenerated the choriocapillaris, which supplies the retina with oxygen and nutrients.
The findings expand on the capability demonstrated in an ongoing, NIH-led first-in-human clinical trial of patient-derived RPE grafts for the dry form of AMD.
The work was supported by the National Eye Institute Intramural Research Program
Source: National Eye Institute (NEI)
Reference:
Gupta R, Bunea I, Alvisio B, Barone F, Gupta R, Baker D, Qian H, Daniele E, Contreary CG, Montford J, Sharma R, Maminishkis A, Singh MS, De Quadros Costa MTM, Kashani AH, Amaral J, Bharti K. “iPSC-RPE patch preserves photoreceptors and regenerates choriocapillaris in a pig outer regina degeneration model”. Published May 22, 2025 in JCI Insight