Diabetic Retinopathy: Hypoglycemia Contributes to Eye Damage and Vision Loss
In a new National Institutes of Health-funded study led by scientists at the Wilmer Eye Institute, Johns Hopkins Medicine researchers say they have determined that hypoglycemia may promote a breakdown of the blood-retinal barrier. An experimental drug, the pharmacologic dual HIF-1 and HIF-2 inhibitor (32-134D), may help to treat the condition.
The research, which investigated the phenomenon in diabetic mice, provides insights into the origin of diabetic retinopathy, specifically in patients with episodes of hypoglycemia.
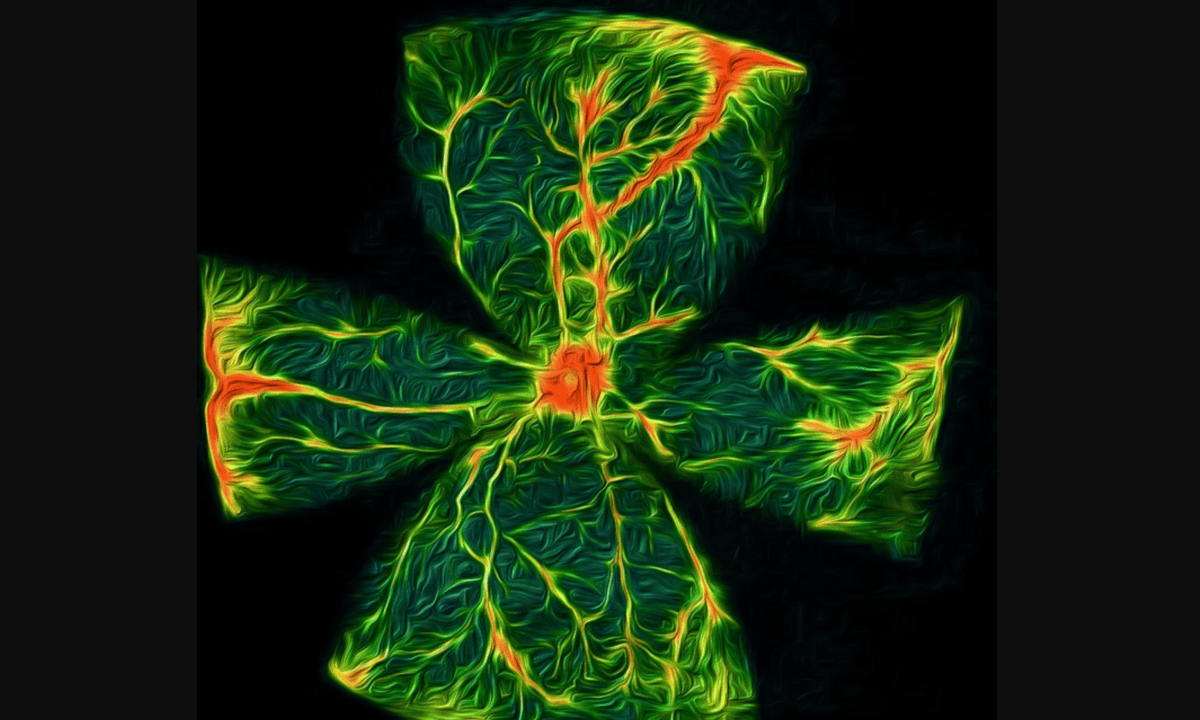
The full study, published in Science Translational Medicine, explains that a specific protein known as hypoxia-inducible factor (HIF) accumulates in certain cells in the retina during periods of low blood sugar.
HIF has been implicated in diabetic retinopathy and other eye diseases before. The protein can trigger a chain reaction, switching on overproduction of other proteins which lead to overgrowth and leakage of blood vessels in the retina. Now, scientists have found that HIF is a player in how the blood-retinal barrier breaks down during hypoglycemia.
Mice with diabetes had higher levels of HIF during hypoglycemia
Researchers tested HIF’s role in hypoglycemia by inducing periods of low blood sugar in mice with and without diabetes. Their experiments showed that mice with diabetes had higher levels of HIF during hypoglycemia, enough to promote the breakdown of the blood-retinal barrier and cause leakage in retinal blood vessels, while mice without diabetes did not experience higher levels of HIF. This breakdown in diabetic retinopathy contributes to irreversible damage to the retina and vision loss.
Therapies targeting HIF will be an effective approach to prevent diabetic retinopathy
The team investigated further by testing an experimental drug known as 32-134D, which inhibits the HIF protein. Some diabetic mice received an injection of 32-134D prior to induced episodes of low blood sugar, and researchers observed lower HIF levels, in turn preventing the expression of proteins that promote the breakdown of the blood-retinal barrier and blood vessel leakage.
“These studies help explain why patients with diabetes who are initially started on tight glucose control, the cornerstone of diabetic management, or those who have high glycemic variability (transient episodes of very low — followed by very high — serum glucose levels), experience worsening of their diabetic eye disease,” says corresponding author Akrit Sodhi, M.D., Ph.D., associate professor of ophthalmology and the Branna and Irving Sisenwein Professor of Ophthalmology at the Johns Hopkins University School of Medicine and the Wilmer Eye Institute. “Our findings underscore why therapies targeting HIF will be an effective approach to prevent or treat diabetic retinopathy.”
Researchers are planning future studies on HIF, the breakdown of the blood-retinal barrier and 32-134D, and hope to conduct clinical studies of 32-134D in patients with diabetic retinopathy.
Chuanyu Guo et al., Hypoglycemia promotes inner blood-retinal barrier breakdown and retinal vascular leakage in diabetic mice.Sci. Transl. Med.17,eadq5355(2025).DOI:10.1126/scitranslmed.adq5355
Source: Johns Hopkins Medicine